Psychosis is a common medical condition that affects about 3% of the population. Psychosis tends to emerge during adolescence and young adulthood, affecting males and females equally. A first episode of psychosis is often frightening, confusing, and distressing for the individual, and upsetting for their family and friends; however, the good news is that it can be treated effectively.
What causes psychosis?
At this time, there are many theories about what causes psychosis, but no definite answers. Psychosis occurs in a variety of mental and physical disorders; therefore, it likely has multiple causes. Biology, stress, and drug use are three of the most common theories.
Biology
Neurotransmitters: There is strong evidence that some psychoses involve a dysfunction in neurotransmitters in the brain. Neurotransmitters are the “chemical messengers” of the brain. They transmit impulses throughout the brain and the central nervous system. Of particular importance is the neurotransmitter dopamine. Most antipsychotic drugs that control the positive symptoms of psychosis also block the transmission of dopamine.
Genetics: Individuals whose close relatives experience psychosis are themselves at increased risk. For example, the risk of developing psychosis associated with Schizophrenia in the general population is approximately 1%, yet the children and siblings of those with Schizophrenia have respective lifetime risks of 13% and 9%.
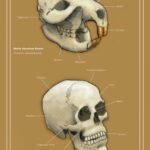
Brain Changes: Changes have been found in the brains of some individuals with Schizophrenia, which appear to have been present since birth or early childhood. Possible causes of the changes include: genetic transmission, abnormal neurodevelopment, and pregnancy or birth complications (e.g. exposure of mother to a virus during the second trimester of pregnancy).
Stress
For some people, psychosis appears to occur primarily in response to stress. In most cases, it is believed that a vulnerability to psychosis combined with stress will lead to psychosis symptoms.
Vulnerability to psychosis is acquired through a genetic predisposition, or as a result of an environmental insult to the brain (brain damage). Vulnerability can be measured by a family history of psychotic disorders, birth complications (e.g. oxygen deprivation of the baby), or brain injuries.
Stresses can be such things as significant life events (e.g. death of a loved one, moving to a new city, etc.), abuse of alcohol and drugs, or stressful living conditions (e.g. high levels of family conflict or financial problems).
The degree of vulnerability varies from person to person. Likewise, the amount of stress that may trigger psychosis likely differs for each individual. For example, a person with a low vulnerability might withstand a large amount of stress without experiencing psychosis, whereas a person with a high vulnerability might only withstand a minimal amount of stress without experiencing psychosis.
Drugs
Psychosis can be induced by drugs or can be drug-assisted. For example, it appears that amphetamines can cause a psychotic episode, while other drugs, including marijuana, can increase a person’s natural vulnerability to psychosis resulting in a psychotic episode.
Is a psychotic person dangerous?
Although some individuals with psychosis may experience mood swings and increased feelings of agitation, they are more likely to present emotional dampening and social withdrawal. While strong delusions and hallucinations may cause a person to react unpredictably or even aggressively, individuals with psychosis are rarely violent, and in fact, they are at much greater risk of causing harm to themselves than to others.
Read more about what causes psychosis.
Common symptoms of psychosis
The most common symptoms of psychosis include disorganized or confused thinking, speaking, and behaviour; changes in mood; delusions; and hallucinations.
Disorganized or confused thinking, speaking, and behavior
Thoughts become confused and seem to either speed up or slow down. Examples of disorganized behaviour include:
- Difficulties performing activities of daily living (e.g. cooking, maintaining hygiene)
- Marked unkemptness, or unusual or inappropriate dress
- Inappropriate sexual behavior
- Unpredictable and unprovoked agitation
- Inappropriate affect (e.g. laughing while describing a personal tragedy)
- Catatonic behavior
The individual experiencing psychosis may have difficulties concentrating, following instructions or conversations, and remembering things.
Changes in mood
An empty feeling marked by a lack of emotions and difficulty expressing feelings. Individuals with psychosis may feel strange and cut off from the rest of the world.
Delusions
Strongly held beliefs which are unusual and unjustified. They are generally organized around one or more of the following themes:
- Persecutory (most common): Belief that one is being followed, tormented, or subjected to ridicule
- Referential (also common): Belief that certain gestures, comments, songs, or other environmental cues are specifically directed toward oneself
- Grandiose: Belief that one has special abilities or “powers”
- Religious: Delusions have religious themes (e.g. receiving orders from God)
- Somatic: Belief that something unusual is occurring in or on one’s body, despite medical evidence to the contrary
- Loss of Control over Mind or Body: Belief that one’s thoughts or body are being controlled by forces or by other individuals. Belief that thoughts are broadcast so others can hear them. A belief that thoughts are being taken out of one’s head or are somehow inserted into one’s brain
- Delusions are considered “bizarre” if they are clearly implausible and are not derived from ordinary life experiences. For example, believing that one’s internal organs have been replaced by someone else’s without surgery would be considered a bizarre delusion, while the belief that one is being followed by the police would be considered non-bizarre.
Hallucinations
Seeing, hearing, feeling, smelling or tasting things that do not actually exist.
- Auditory hallucinations are the most common. They are usually experienced as voices that are perceived as distinct from the individual’s own thoughts.
- Visual hallucinations are often of a disturbing and intrusive type.
Phases of psychosis
There are three phases involved in psychosis: the prodromal phase, the acute phase, and the recovery phase.
Prodromal phase
Often not clear until after positive symptoms emerge:
- Something isn’t quite right
- Not definite
- Negative symptoms emerge (e.g. loss of motivation, decreased range of facial expression)
- Become more isolated
- Drop out of activities
- Less concern with personal appearance
- Unusual preoccupations such as religion, politics, or science fiction
Acute phase
Characterized by the experience of intense symptoms (e.g. hallucinations, delusions, thought disorder). Symptoms become obvious to others. These types of symptoms are often referred to as positive symptoms.
- Usually in this phase that treatment begins
- Early intervention leads to quicker recovery, better outcomes
Recovery phase
Gradual return to normal functioning:
- Often difficult to come to terms with what has happened
- Sometimes a grief reaction follows, due to the losses that occur as a result of the illness
- Confidence and self esteem may be affected
- Sometimes there is a loss of faith in one’s own judgment and perceptions